A 65 years old male patient with SHORTNESS OF BREATH since 6 days….
Date:3/12/22
This is an online e-log book to discuss our patient de-identified health data shared after taking his / her / guardian's signed informed consent. Here we discuss our individual patients' problems through a series of inputs from the available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based information.
This E blog also reflects my patient-centered online learning portfolio and your valuable input in the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and coming up with diagnosis and treatment plans. is an online e-log book to discuss our patient's de-identified health data shared after taking his / her / guardians' signed informed consent. Here we discuss our individual patients' problems through a series of inputs from the available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based information.
CASE REPORT
A 65 years old male patient who is a resident of
Choutuppal was once a farmer by occupation
(stopped working 6 years ago) came to Medicine
OPD with chief complaints of ;
(Date of history taking and examination - 2/12/22)
> Lower Abdominal pain for 6 days
> Shortness of breath for 6days
HISTORY OF PRESENTING ILLNESS :
The patient was apparently asymptomatic 25 years ago, then he developed cough which was blood stained for which he was diagnosed with Tuberculosis and was on Anti tubercular therapy for 6 months then after he was said that he is free from disease.
2 years back he started having Shortness of breath (Grade 2) , which was insidious in onset and relieved temporarily on medication (Drug & Dosage unknown).
6 months ago he again developed shortness of breath (Grade 2) which was insidious in onset and he was taken to higher centre, where he was prescribed a medication that he used only on the aggravation of shortness of breath.
Then after 5 months ago he suffered from an accident which was associated with fracture of left tibia and left tibia, for this he was managed with POP casting (45 days) and supplementation of calcium tablets (Dose: 500mg).
Also 6 days ago he also developed diffuse pain over the abdomen which was insidious in onset, non radiating and was subsided now.
NO H/O fever with chills and rigor
NO H/O anorexia, nausea, vomiting
NO H/O loss of weight
Then 6 days ago he developed shortness of breath of grade 3, which was insidious in onset and relieved temporarily on medication ( Drug not known).
There is also a history of diarrhoea since 2 days.(under evaluation )
PAST HISTORY :
History of Pulmonary Tuberculosis 25 yrs ago.
Patient is conscious, coherent and co operative well oriented to time place and person.
Moderately built and nourished
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - No palpable lymph nodes
Edema - absent
Temperature - afebrile
BP - 120/80 mmHg
RR - 24 cpm
PR - 78 bpm
SpO2 - 96?????
RESPIRATORY SYSTEM :
INSPECTION :
Shape of chest - Elliptical, B/L symmetrical.
Trachea position central
Chest movements - Abdomino thoracic type with no involvement of accessory muscles
No scars over the chest
PALPITATION :
(All inspectory findings are confirmed)
No tenderness
Expansion of chest equal in all planes
PERCUSSION :
Resonant tone all over the chest except infra axillary area.
AUSCULTATION :
Bilateral vesicular breath sounds heard in all areas except the left infra axillary where there is decreased breath sounds.
PER ABDOMEN :
INSPECTION :
(All 9 regions are examined)
Shape - scaphoid
Abdominal distension - absent
Skin over the abdomen - normal
No engorged veins
PALPATION :
No tenderness
No hepatomegaly and splenomegaly
PERCUSSION :
Normal
AUSCULTATION :
Bowel sounds - heard
CARDIOVASCULAR SYSTEM :
INSPECTION :
No visible apex beat / pulsations
No scars, engorged veins
PALPATION :
Apex beat diffuse
No palpable murmurs / thrills
AUSCULTATION :
S1 and S2 heard ; No murmurs.
PROVISIONAL DIAGNOSIS :
Cor Pulmonale Heart failure ( mid range preserved ejection fraction EF 52%) With anemia under evaluation With Chronic Kidney disease (heart failure and cystic kidney disease) With history of pulmonary tuberculosis 25 years ago.
INVESTIGATIONS :
29/11/22
30/11/22
1/12/22
TREATMENT :
Head end elevation up to 30 degrees
supplementation if spo2
<90%
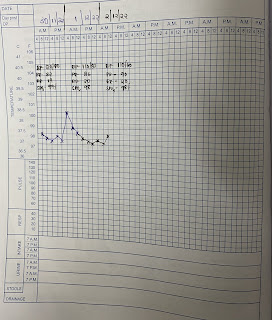
MONITOR 4- hrly
NEB - SALBUTAMOL 4 hrly
FEVER CHART 4 th hrly
InJ LASIX 4O mg
ORS sachets

























Comments
Post a Comment